Abstract
Nanotechnology ushered the field of medicine in to a new era. Miniaturization, increased surface area, and the unique physicochemical properties in the nano dimension were explored for new applications. Pharmaceutical industry picked up the technology and early success came fast for oral drug delivery through improvement in dissolution properties of the active molecules. Many products were launched using the nanocrystal technology on the oral side. Further development of polymeric nanoparticles led to wide spread research of nanocarriers for parenteral delivery. While considerable efforts have gone in the last two decades for testing nanoparticles for tumor targeting, delivery into tumors has remained challenging and suboptimal. Inadequate in vivo models that didn't accurately reflect the age and vascularity of human tumors, and inability to reproducibly target therapeutic drugs to the tissue of interest due to intrinsic biodistribution of the particles and hence side effects, limited the number of studies that advanced to the clinic. Our article addresses the questions commonly asked by scientific researchers in nanomedicine: “Has nanoparticle technology yielded on its initial promise that scientists predicted towards improving therapeutic index and avoid toxicity by delivering molecules to target tissues or was it more of wishful thinking that had several roadblocks?” We answer this question by linking the relevance of nanoparticles to cancer immunotherapy. The advent of immunotherapy has begun to show the potential applicability of nanoparticles in a different light, to target the immune system. In this approach, nanoparticles may positively influence the immune system rather than create the targeted “magic bullet”. Utilizing the intrinsic properties of nanoparticles for immune targeting as opposed to targeting the tumor can bring about a positive difference due to the underlying complex cancer mechanisms that can potentially overlap with the heterogeneous biodistribution of nanoparticles towards improving the acquired and innate immune responses. In this review, we have followed the progress of nanotechnology in pharmaceutical applications with key insights from oral and parenteral drug delivery, and how to modify our thinking to better utilize nanoparticles for immuno-oncology. In contrast to conventional “local” tumor targeting by nanoparticles, we propose a new mechanism whereby nanoparticles trigger priming of the T cells towards tumor destruction. The heterogenous biodistribution of nanoparticles lends itself to stimulating immune cells systemically in a “global” manner and with the right therapeutic combinations will be able to trigger tumor antigens to continually activate, retain memory effects and destroy tumor cells.
Conclusions
With the advent of nanotechnology in the last few decades, the projected future of new applications towards healthcare is expected to offer many improvements for human life and drug delivery in particular. However, if nanomedicines are to realize their full potential, a few impediments must be addressed right now. For drug delivery, for example, a deeper understanding of the biology and development of appropriate disease models and the interaction of cells with nano- carriers is needed, PK characteristics and the fate of nanocarrier in vivo is also critical to develop PK/PD correlations for immunotherapy while using nanoparticles.
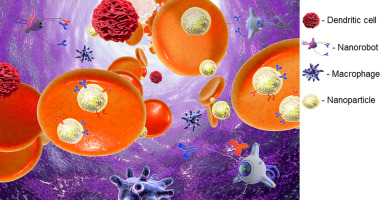
The winner of the 2016 Nobel Prize in chemistry, Dr. Bernard L. Feringa, envisioned many possible biomedical applications for mole- cular machines, saying “It's a bit early days, of course, but once you are able to control movement, all sort of things are possible. Think about tiny little robots that the doctor would inject into your bloodstream, and that would go search for a cancer cell or deliver a drug” [91]. We hope that nanotechnology will disrupt cancer immunotherapy with new treatment possibilities very soon in the near future....
Recommended for you